Volume 11 Issue 1 pp. 97-118 • doi: 10.15627/jd.2024.6
Exploring Methodological Considerations: A Literature Review on How Lighting Affects the Sleep and Cognition in Healthy Older Adults
Mahya Fani,∗ Nina Sharp
Author affiliations
The Design School, Arizona State University, Tempe, USA
*Corresponding author.
mfani1@asu.edu (M. Fani)
nina.sharp@asu.edu (N. Sharp)
History: Received 19 March 2024 | Revised 2 May 2024 | Accepted 18 May 2024 | Published online 6 june 2024
Copyright: © 2024 The Author(s). Published by solarlits.com. This is an open access article under the CC BY license (http://creativecommons.org/licenses/by/4.0/).
Citation: Mahya Fani, Nina Sharp, Exploring Methodological Considerations: A Literature Review on How Lighting Affects the Sleep and Cognition in Healthy Older Adults, Journal of Daylighting 11 (2024) 97-118. https://dx.doi.org/10.15627/jd.2024.6
Figures and tables
Abstract
The impacts of lighting conditions on human circadian rhythms, sleep quality, and cognitive performance have been extensively investigated in the past two decades; however, these studies have yielded inconclusive and variable outcomes. For older adults who are at a higher risk of developing serious physiological and mental illnesses, such as Alzheimer’s or dementia, light therapy has emerged as a low-risk intervention to improve sleep quality and cognitive function. Nevertheless, the optimal methodology for evaluating the efficacy of light therapy in older adults remains unclear. This review has been conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and critically analyzes methodologies in previous studies on lighting's impact on sleep and cognitive performance in healthy older adults, focusing on how these approaches affect the findings. The review is structured into six domains: study setting and type, participant characteristics, lighting conditions, study design, sleep quality evaluation methods, and cognitive performance evaluation methods. Diverse study designs, methods, and population characteristics have influenced the outcomes. Bright light, applied from early morning to early evening, has been shown to enhance sleep and cognitive functions, notably working memory and concentration. It also benefits from dawn simulation throughout the day, which regulates circadian rhythms and improves sleep quality, although the ideal timing is yet to be determined. Intense short-wavelength lights and strong placebo conditions can counteract these positive effects, and using bright light in the evening may impair sleep and indirectly worsen cognitive performance in older adults. Further real-world experimental studies on this demographic, meticulous study designs, a combination of objective and subjective evaluation methods, and comprehensive reporting of lighting interventions are crucial for identifying the optimal lighting design approach for this population.
Keywords
Lighting, Healthy older adults, Sleep quality, Cognitive performance
Nomenclature
| AD | Alzheimer’s Disease |
| ADRD | Alzheimer’s Disease Related Dementia |
| WHO | World Health Organization |
| ipRGCs | Intrinsically photosensitive retinal ganglion cells |
| CCT | Correlated Color Temperature |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| EXP | Experimental Study |
| OBS | Observational Study |
| COR | Correlational Study |
| RCT | Randomized controlled trial |
| EEG | Electroencephalogram |
| ECG | Electrocardiogram |
| PGS | Polysomnography |
| KSS | Karolinska Sleepiness Scale |
| KDT | Karolinska Drowsiness Tests |
| SSS | Stanford Sleepiness Scale |
| KLT-R | Konzentrations-Leistungs -Test |
| PVT | Psychomotor Vigilance Task |
| KSSCLE | Karolinska Sleepiness Scale, Core Level Effort |
| MMSE | Mini mental state exam |
| PSQI | Pittsburgh sleep quality index |
| MEQ | Morningness- Eveningness questionnaire |
| SAQ | Sleep Assessment Questionnaire |
| ESS | Epworth Sleepiness Scale |
| VAS | Visual Analogue Scale |
| NPCRA | Non-parametric circadian rhythm |
| OSQ | Oviedo Sleep Questionnaire |
| PROMIS_SD | PROMIS Sleep Disturbance |
| PROMIS_SR | PROMIS Sleep- Related Impairments |
| DSST | Digit Symbol Substitution Test |
| TMT-A, TMT-B | Trail-Making Tests |
| EML | Equivalent Melanopic Lux |
| MEDI | Minimum Melanopic EDI |
| CS | Circadian Stimulus |
| SPD | Spectral Power Distribution |
| SWA, SWS | Slow wave activity/ sleep |
1. Introduction
As individuals age, attaining quality sleep and maintaining an appropriate level of cognitive stimulation becomes increasingly crucial to enhancing overall health and well-being. Cognitive performance, which encompasses an individual’s capacity to interact with (process, retain, and recall) information, make decisions, and perform tasks [1,2], is influenced by several factors. Notably, emerging research highlights the significant role of sleep quality and human circadian rhythm as vital biological determinants impacting cognitive performance, memory, and processing speed [3–5]. Previous studies have reported reduced sleep quality, inefficient cognitive performance, and circadian rhythm disruption in the aging population [6–9]. These age-related issues increase the risk of serious neurodegenerative diseases, such as Alzheimer’s Disease (AD) and Alzheimer’s Disease Related Dementia (ADRD) [10], which are growing concerns among the older adults. Maintaining a healthy lifestyle, including proper sleep hygiene, and circadian lighting, is essential in seeking preventive solutions for AD, and ADRD.
It is important to note that the relationship between sleep and cognitive performance is complex and multifactorial. While disturbed sleep can have negative impacts on cognitive functions and accelerate cognitive declines in older adults, the reverse is also true, as cognitive decline can contribute to poor sleep quality. Research shows that individuals experiencing cognitive decline may have difficulties with memory, attention, and executive functions, which can disrupt their ability to initiate and maintain sleep [11,12]. Moreover, behavioral and psychological changes associated with cognitive decline, such as anxiety, depression, and agitation, can also contribute to sleep disturbances [4,13,14].
Given the rapidly growing aging populations in most countries, the world population is becoming proportionally older [15]. This ongoing demographic shift in developed countries like the United States is increasingly challenging their health infrastructures and highlights the urgent need to adapt and ensure supportive living environments for the growing older adult population [16]. The World Health Organization (WHO) estimates that the number of older adults diagnosed with dementia will triple from around 55 million worldwide in 2023 to 160 million by 2050 [17,18]. This surge in dementia and Alzheimer’s disease rates highlights the need for further research and exploration, emphasizing the importance of preventative and effective solutions.
Recent research indicates that well-designed lighting can significantly influence sleep and cognitive performance in healthy older adults, potentially reducing the risk of age-related illnesses, including Alzheimer’s and dementia [18–20]. Appropriate lighting plays an essential role in the health and well-being of individuals [21–24] by regulating bodily functions and the secretions of hormones, such as melatonin [25,26]. Melatonin hormone is released in a 24-hour cycle depending on the amount of light received by the human eye [27–30]. In regular sleep-wake cycles, the melatonin hormone level is at its highest during darkness in order to promote healthy sleep and is at its lowest level during daylight in order to increase alertness [28]. Disruptions of these rhythms, caused by aberrant light exposure that doesn’t follow the natural light/ dark cycle, affects human sleep, cognition, and alertness [21,27,31].
Recent research indicates that well-designed lighting can significantly influence sleep and cognitive performance in healthy older adults, potentially reducing the risk of age-related illnesses, including Alzheimer’s and dementia [18–20]. Appropriate lighting plays an essential role in the health and well-being of individuals [21–24] by regulating bodily functions and the secretions of hormones, such as melatonin [25,26]. Melatonin hormone is released in a 24-hour cycle depending on the amount of light received by the human eye [27–30]. In regular sleep-wake cycles, the melatonin hormone level is at its highest during darkness in order to promote healthy sleep and is at its lowest level during daylight in order to increase alertness [28]. Disruptions of these rhythms, caused by aberrant light exposure that doesn’t follow the natural light/ dark cycle, affects human sleep, cognition, and alertness [21,27,31].
Recent scientific discoveries have identified intrinsically photosensitive retinal ganglion cells (ipRGCs) as a novel photoreceptor that plays a critical role in regulating blood circulation, sleep quality, alertness, and circadian rhythms, which, in turn, affects various cognitive processes, such as memory and attention [6,32,33]. Aging is associated with physiological and psychological changes that disrupt the body’s response to light cues, making it more difficult for older adults to maintain a healthy circadian rhythm [34]. These age-related changes can negatively affect visual functions and the optical system, bringing about yellowing lenses’ pigmentation, reducing pupil diameter and night-dark cycle adaptation, and damaging contrast sensitivity [35,36]. The negative implications of this reduced ability for older adults to absorb light is compounded by the fact that the amount of light a 20-year-old individual receives is three times higher than a 60-year-old individual [37]. This reduced sensitivity to light cues makes older adults more vulnerable to the effects of lighting on their cognitive performance and sleep quality.
Different characteristics of light, including intensity, spectrum (often indicated as Correlated Color Temperature [CCT]), and duration and timing of exposure, cause significant influences on human sleep, and cognitive performance [33,38–42]. The ipRGCs are more sensitive to the blue part of the light spectrum, which is in short wavelengths. The highest sensitivity has been reported for 470-480 nm wavelength [43,44]. Light exposure, particularly in the blue spectrum, can suppress the production of the hormone melatonin, potentially disturbing sleep initiation and quality, which in turn may impair cognitive functions such as attention, memory, and executive abilities [45].
Previous studies demonstrated the therapeutic benefits of lighting in improving the psychophysiological health and regulating the rhythmicity of older adults, who are among the vulnerable population [45–49]. Promising evidence suggests that lighting interventions can delay or prevent the onset of dementia and Alzheimer’s disease and promote healthy aging [48,50,51]. However, further research is required to identify the optimal lighting interventions for improving sleep and cognitive performance in older adults.
Previous reviews explored the effects of light interventions on sleep, circadian rhythms, behavioral and psychological issues in older adults’ populations, revealing inconsistencies in study outcomes. However, most of these reviews are focused on older adults with dementia or Alzheimer [18,52–54]. This gap in research is critical for developing preventive strategies aimed at preserving cognitive health in the aging population, thereby delaying or preventing the onset of Mild Cognitive Impairment (MCI), Alzheimer or dementia. Such measures are essential for promoting healthy aging and reducing the societal burden associated with these conditions. This review aims to provide a comprehensive understanding of the role of lighting in healthy aging. It will specifically assess how various studies have administered lighting exposure, including aspects such as timing, duration, correlated color temperature (CCT), and intensity. Additionally, it will examine study designs, participant characteristics, and methods of sleep and cognition evaluation, focusing on how these methodological aspects influence the outcomes of the studies (Fig. 1). The ultimate goal is to build a comprehensive foundation for future lighting research that contributes to the promotion of healthy aging strategies.
2. Methods
This review has been conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [55], which includes recent advancements in methodologies for identifying, selecting, evaluating, and synthesizing studies.
Multiple databases were comprehensively searched for relevant topics on the research area. Four main databases—including Science direct, PubMed, and Scopus were searched for published papers after 2010 to ensure that the selected research encompasses the latest technological advancements and developments in the field, providing a comprehensive and up-to-date understanding of the topic. Additionally, Google Scholar was specifically queried for the first 100 results to ensure comprehensive coverage of all pertinent literature. An advanced search was employed within these databases using the keyword reported in Table 1. Only papers written in English were considered. The keywords have been categorized in four-word groups: study population, lighting condition, target variables, and target population health and well-being condition. The studies had to investigate the influence of either daylight or artificial light on healthy older adults’ sleep, and cognitive performances, or a combination of these parameters. The searching and screening strategies were divided into four parts: identification, screening, eligibility, and inclusion. The following information was extracted from the reviewed papers: number and characteristics of participants and the considered inclusion/exclusion criteria, study design, different types of lighting condition, including intervention and control condition, study setting, measurement methods, and reported study findings.
A detailed overview of the screening process and the number of initial hits and identified papers from each database is reported in the PRISMA Flow diagram in Fig. 2. At the first stage, the keywords were connected to each other using the Boolean operators “AND” and “OR” to search each database and find the most relevant targeted papers for review. A total of 1,495 papers were reached during the initial search according to the keywords and the removal of duplicate studies; then, the number of papers was reduced to 148 papers after the title and keyword screening step. As the focus of this literature review is on the effectiveness of lighting conditions in preventing serious health issues from developing in healthy older adults, studies that included participants with Alzheimer’s, dementia, MCI, or any mental or physiological health issues, such as visual impairment (cataract) have been excluded. Our search strategy was specifically designed to focus on studies involving older adults. We included papers that explicitly mentioned older adults in their research scope. If studies included both adults and older adults, we only considered and reported the findings related to the older adult population.
In the next step, abstracts of the selected papers were screened. Studies not including lighting aspects and only covering aging, sleep, cognition, and circadian rhythms of older adults were excluded. Observational and interventional studies were included while review studies were excluded. Studies not conducting data collection, either through field measurement or from a lab experiment, and only covering the theoretical aspects of lighting and daylighting and its influence on older adults sleep quality and cognitive performance were excluded. A list of references of the included studies that were conducted after 2010 was also screened and resulted in 7 additional studies being added to the literature review. Finally, after the full process of screening, 33 papers were selected and reported in the current literature review.
3. Results
This review critically assesses the existing scientific literature on how different lighting conditions affect the sleep patterns and cognitive abilities of healthy older adults. It includes an extensive range of studies, covering both experimental interventions in lighting and observational studies that examine baseline lighting conditions without any modifications. The studies included in this review are divided into two primary categories: those conducted in controlled laboratory settings and those carried out in real-world, field-based environments. For a detailed analysis, participant demographics, study designs, specific lighting conditions, and evaluation methods are summarized in Tables 2 and 3. This classification forms the initial approach to the methods utilized in the studies.
The structure of the results section is meticulously organized to facilitate a comprehensive review. It includes details on study settings, types, participant characteristics, study designs, and lighting conditions. Furthermore, the impact of these lighting conditions on sleep quality, including the sleep assessment methods used, is extensively reviewed. Additionally, the influence of lighting on cognitive performance is examined, with various tests employed to assess different cognitive domains. The findings are systematically reported under two subsections: lab-based studies and field-based studies.
3.1. Setting and study type
Studies are organized in two categories: lab-based and field-based. While lab-based studies provide a controlled environment with standardized conditions, they lack the ability to investigate the impact of lighting design in real-world settings. Experimental (EXP) studies manipulate independent variables to observe their effects on a dependent variable, while observational (OBS) and correlational (COR) studies measure variables without manipulating them to describe natural phenomena and examine relationships between variables. As reported in Tables 2 and 3, among the 33 studies reviewed, 13 were lab-based, 19 were field-based, and 1 study was conducted in both settings. All of the lab-based studies reviewed in this research paper were experimental. Among the 20 field studies, 11 of them were observational and correlational and nine of them were experimental and examined participants in their natural living environment. However, these studies were subject to limitations, such as the lack of control for variables (e.g., humidity, temperature, and interior design parameters affecting circadian lighting within the space). Field-based experimental studies also mentioned limitations, such as small sample size [7,66,82,85], gender [75] , living status of the participants [31], and seasonal differences during the period of the data collection [31,81]. Some of the experimental field-based studies also acknowledged potential biases in their results due to older adult enthusiasm for the new lighting system in their living environment, their participation in scientific research, or compensation [31,37]. As the focus of this study is on healthy older adults, most of the field studies were conducted in residential spaces [74,81,86] or health care facilities [77,78].
3.2. Participants characteristics
This section provided a review of the study participants’ characteristics and the inclusion/exclusion criteria being used in the literature. Taking all the reviewed studies into account, the participants average age was 69.9 years, with three studies not mentioning the mean age of the participants. Two of the studies did not mention the participants age and only mentioned the older adult population [70,84]. Three of the studies, although, did not mention the average age, they did mention that participants’ ages were above 50 [72], 65[74], and 70 [68] years old, respectively. Majority of the studies had 10 to 30 participants and there are a few studies that had a very short sample sizes of less than 10 participants [72,75,84].
The inclusion and exclusion criteria for the study participants varied across different studies. However, many common themes can be identified. In general, the inclusion criteria across the studies involved assessing participant medical and psychological health, sleep quality, and cognitive performance. Most studies screened participants for medical, psychological, and ophthalmological disorders, using questionnaires, physical examinations, and structured interviews with health-care professionals (see Tables 2 and 3). In two studies an overnight polysomnography was performed to screen participants for sleep apnea and periodic limb movement disorder before the actual study started [7,67]. The participant sleep quality was evaluated using different questionnaires, such as the Epworth Sleepiness Scale (ESS), Morningness- Eveningness Questionnaire (MEQ), and the Pittsburgh Sleep Quality Index (PSQI) [61,64,66]. Participants were also required to maintain a regular sleep-wake schedule for a specified period before the study to ensure stable circadian entrainment. In some of the studies they were requested to abstain from excessive alcohol and caffeine consumption to maintain a regular sleep-wake cycle for at least one week before the study start time [62,74,77]. Compliance was monitored through self-reported sleep logs and wrist actigraphs. One study also conducted the Alcohol Use Disorders Identification Test (AUDIT) [66]. Additionally, some research studies required participants to be English-speaking older adults. Only one study had inclusion criteria of at least 12 years of education for participants [62]. The majority of the studies did not specify the participants' nationalities, leaving a gap in demographic information.
The exclusion criteria for the studies were mainly aimed at controlling for variables that could impact sleep quality. For example, some studies excluded participants with sleep-related breathing disorders, restless leg syndrome, psychiatric illness, substance abuse, high BMI (body mass index > 25), color blindness, and ocular conditions that could interfere with bright light exposure [62,65]. Researchers also mentioned that participants with visual impairments had been excluded except for those with myopia or hyperopia [65], which could be corrected by wearing contact lenses. One study excluded participants who reported a history of head or eye injury [74]. Although most of the studies evaluated the sleep parameters to ensure the participant sleep quality met the requirements for eligibility, some did not have any inclusion/exclusion criteria based on sleep [37]. Moreover, two studies included only participants with a sleep complaint—meaning those waking up too early or having frequent nighttime awakenings [7].
A few studies mentioned the use of light therapy as exclusion criteria for selecting the target participants. These studies also mentioned the importance of not spending more than five hours of waking time per day outside the interior spaces for participants [31,37]. One study highlighted how it considered the records of evening light measurements in two 48-hour sessions as an inclusion criterion for participants [73].
Finally, most studies included participants who were in good physical and psychological health, had normal visual acuity, and had no history of substance abuse or medication use that would affect sleep. Overall, the studies’ inclusion and exclusion criteria appear to be designed to control for variables that could impact sleep quality, cognitive performance, and other factors that could influence the results. The studies’ specific requirements, however, varied somewhat based on the research question and objectives.
3.3. Study design
The study design is the most important component of any research study, as it establishes the validity and reliability of the findings. Tables 2 and 3 present the findings of a comprehensive review of 33 studies, revealing that 21 of them were experimental. However, a considerable number of these studies were conducted in laboratory settings and failed to account for the impact of real-world environments on the generalizability of their findings.
Among 13 lab-based studies—all of them experimental—six of them employed a within-subject crossover study design to evaluate the effects of the different light conditions for each participant [60,61,63,65–67]. These studies applied either a counterbalancing technique to control for order effects or random assigning technique to control for individual differences. The rest of the lab-based studies had randomized controlled trial study design, which aimed to determine the effectiveness of a particular lighting condition by comparing findings between the intervention group and the control group—which received either no treatment or a placebo. It is important to note that because of the limitations of the lab-based studies, most of the them applied short durations of light exposure. For example, as shown in Table 2, in studies [58] and [66], participants underwent three and two nights of lighting exposure, respectively. Therefore, these studies lack the long-term influence of lighting on the tested variables.
Among 20 field-based studies, nine of the studies were experimental. Six of the studies employed randomized controlled trial study design [69,70,74,80,83]. One study had a quasi-experimental design with pretest and posttest measures where participants were not randomly assigned to different groups. Instead, researchers compared the dependent variables before and after the intervention and compare these to measurements from a control group [82]. This method allows researchers to infer changes potentially caused by the intervention, though it may be more susceptible to confounding variables than a randomized controlled trial. One experimental pilot study employed a single-arm, open-label longitudinal design in which participants were aware of the treatment being given [84]. Most of the correlational and observational studies conducted in the field were cross sectional studies and collected data at a single point in time to find the correlations among variables [68,71,72,75,76,79,87]; some had repeated measures and before-after trials to measure the changes in variables over time [77,78,87]. Overall, experimental, observational, and correlational studies have their strengths and limitations in studying the appropriate lighting exposure and its impacts on health and well-being. The reviewed literature indicates that studies incorporating randomized trials reported more significant outcomes compared to those employing different methodologies. Additionally, it was observed that the majority of experimental design studies were conducted within laboratory settings. In contrast, field studies predominantly adopted observational or correlational approaches, focusing on baseline lighting conditions without any lighting interventions.
3.4. Lighting condition
Lighting conditions play a crucial role in determining the physiological and psychological responses of individuals. Experimental studies consider various lighting conditions, including both a baseline lighting condition and an interventional lighting condition and involve assigning participants (randomly or not randomly based on the study design) to different lighting conditions and measure their sleep and cognitive performance. On the other hand, observational studies involve observing and measuring variables without manipulating them, such as observing the ambient lighting condition in the space and measuring the sleep and cognitive performance of individuals who spend time in that environment. Correlational studies also involve measuring the significance and the relationship between the variables, including lighting and sleep/cognitive performance without manipulating them.
As shown in Tables 2 and 3, among the 33 selected studies, 24 studied focused on the influence of different interventional lighting conditions on sleep or/and cognitive performance. The remaining nine studies observed the baseline illumination condition. Different studies considered various aspects of lighting conditions. These aspects include the timing and duration of light exposure, light intensity, and CCT, which are detailed below. Subsequent sections of this paper will further explore the impact of these lighting conditions on sleep and cognitive performance of healthy older adults.
3.4.1. Timing and duration
Timing of light exposure is an important aspect of lighting conditions [38]. Researchers have found that exposure to light during certain times of the day can have different effects on human physiological and psychological responses. Among the experimental studies that explored various interventional lighting conditions, variations can be seen in terms of lighting exposure duration and timing. Four of the reviewed studies applied the interventional lighting condition during morning time [62,70,79,82], three during evening time [7,56,73], and five studies applied the interventional lighting condition during the night and midnight [57–59,66,87]. The duration of the light exposure intervention also varied widely across studies, ranging from 30 minutes to several hours during day and night. For example, while [66] considered the influence of 30 minutes of light exposure at night on older adults, another study investigated longer lighting exposure from morning to the evening time for around 6 hours [83].
Two different interventional lighting conditions were explored by researchers in a study conducted over an eight-hour exposure period from 10 p.m. to 6 a.m. [58]. Additionally, another study [57] examined both a controlled condition and an intervention lighting condition for a four-hour duration from 10 p.m. to 2 a.m. One study also considered 40 hours of wakefulness while participants underwent three lighting treatment conditions [64].
3.4.2. Intensity and CCT
Indoor artificial lighting conditions considered in the reviewed studies varied widely, including bright light, dim light, polychromatic white light, standard white fluorescent light, blue-enriched and blue suppressed light, dawn simulation lighting condition, complete darkness, and various other interventional and baseline lighting conditions. Researchers have found that light intensity levels and different color temperatures can affect physiological and psychological responses and impact sleep and cognitive performance. In defining various interventional lighting conditions, 11 out of the 33 reviewed studies considered both intensity and color temperature [37,64,65,83]. The remaining studies considered either a baseline condition [75–77] or an interventional lighting condition with variations in light intensity only [62,74,82,85], without examining the effects of CCT.
Studies considered various lighting intensities ranging from complete darkness (lux< 0.05) to bright light with 10,000 lux. These studies defined typical lighting and bright lighting conditions differently based on the context of the study. For example, [82] examined the influence of 90 minutes of light exposure at 100 lux (typical lighting condition) to 1,000 lux (bright lighting condition) in the morning. Another study investigated a dawn simulation with a range of 0 to 250 lux in the morning [66], while in [60], researchers examined four lighting conditions ranging from 300 to 2,700 lux as a bright light condition. Additionally, a different study defined their typical lighting condition as 500 lux to 1,000 lux and their bright light condition as 3,000 lux to 5,000 lux [62].
Among the studies that considered CCT of the light in combination with various light intensities, the typical CCT level was between 2,700 K to 17,000 K. For example, [37] considered the interventional condition with a high lighting illumination of 500 lux in the morning with CCT of 6,500 K (blue-enriched) in the morning followed by gradually lower illuminance levels and CCT throughout the day, reaching 100 lux and 2,700 K in the evening. This study defined the control lighting condition with the same range of illuminance levels and constant CCT of 2,700 K during the day. However, another study conducted by [83] considered the placebo condition with 300 lux and CCT of 3,500 K and the interventional condition with light intensity ranging from 80 lux to 1,000 lux and CCT ranging from 2,700 K to 5,000 K.
While multiple studies have highlighted the beneficial effects of lighting exposure on sleep and cognitive performance, this review indicates a lack of consistent patterns among the previous studies. The characteristics of lighting conditions varied across studies, with differences in exposure times, durations, intensity levels, and correlated color temperatures (CCT). These variations led to inconsistent results regarding their effects on both sleep and cognitive performance.
3.5. Lighting, sleep, and evaluation methods
Among the reviewed studies, 29 of them assessed the effects of either baseline lighting exposure, or examined the influence of interventional lighting schemes with varying illumination levels, CCT, and the timing of exposure on sleep patterns in healthy older adults. While the primary focus of the search was on sleep-related parameters, studies that also assessed variables, such as alertness, sleepiness, and circadian rhythm, were included as they are closely related to sleep.
The studies utilized various subjective measurement methods to assess sleep and alertness, including the Pittsburgh Sleep Quality Index (PSQI) for sleep quality and patterns evaluations, Karolinska Sleepiness Scale (KSS) and Stanford Sleepiness Scale (SSS) for degree of sleepiness, and Morningness- Eveningness Questionnaire (MEQ) for individuals’ circadian preference. Other less commonly used subjective measures included Epworth Sleepiness Scale (ESS) for daytime sleepiness, Karolinska Drowsiness Test (KDT) for drowsiness levels, Karolinska Sleep Diary (KSD), Oviedo Sleep Questionnaire (OSQ), and Sleep Assessment Questionnaire (SAQ) for sleep habits and disorders, Slow wave activity/sleep (SWA, SWS), KSSCLE (Karolinska Sleepiness Scale, Core Level Effort), PROMIS Sleep Disturbance (PROMIS_SD), and PROMIS Sleep- Related Impairments (PROMIS_SRI). These mentioned methods of measurement were applied either before, during, or after the lighting intervention, when participants were exposed to light. Objective measurements of sleep and alertness were also employed in several studies, both in laboratory and field settings. Polysomnography (PSG), including electroencephalography (EEG), was used in laboratory settings, while actigraphy was the most commonly used field measurement method. Melatonin levels were assessed through saliva and blood sampling in some studies to assess circadian rhythm. Only a few studies used alternative objective measurement devices, such as Emfit bed mat sensors [84] or Dimesimeters [72]. Table 4 presents a summary of the most commonly used subjective and objective methods for evaluating sleep. These studies are divided in two categories of laboratory-based and field-based studies which are explained in detail in the following sections.
3.5.1. Lab-based studies
Among the 33 studies reviewed, 13 were conducted within a controlled laboratory environment. A majority of the studies (11 out of 13) were experimental and considered interventional lighting impacts. The two other papers were observational and correlational and considered the baseline lighting condition and the correlations between light, sleep, and alertness.
Different methods of evaluation, including objective and subjective techniques, were employed to study the impact of lighting on sleep parameters and alertness. This review revealed that most of the studies that only employed subjective techniques for assessing sleep quality parameters, such as questionnaires and surveys, found no influence of lighting on improving sleep quality and alertness among healthy older adults. One within-subject balanced crossover study conducted by [60], investigated the effects of four different lighting conditions, ranging from 300 lux to 2700 lux, on two groups of young and older adults during four laboratory visits. Sleep quality was assessed by KSS and results indicated no impact of the lighting conditions on sleep and subjective alertness. In another between-subject randomized controlled study by [58], the influence on sleep quality caused by exposure to a bright night light of 3000 lux was compared to that caused by a room light exposure of 300 lux from 10 p.m. to 6 a.m. The SSS was used and the results indicated no difference in older adults’ sleep quality when being exposed to different lighting conditions at night.
On the other hand, studies that used a combination of objective methods—including actigraphy and polysomnography—and subjective methods, such as SSS and KSS (two of the most common methods in lab-based studies) found more significant influence of appropriate lighting design on improving sleep quality and alertness. For example, in an experimental balanced crossover study conducted by [56], the influence of two different evening light exposures, including polychromatic blue-enriched white light or standard white fluorescent light were studied. Researcher analyzed data collected by KSS, KDT, and wake and sleep EEG data for sleep quality and evening alertness. They found that evening light exposure can improve subjective and objective alertness and shift the timing of circadian rhythm among older adults. It could also benefit older adults’ early evening sleepiness without negatively impacting the subsequent sleep episode. Another study was conducted to examine the impact of different light interventions on sleep deprivation [61] on two groups of participants, consisting of 26 young adults and 12 older adults. Over a period of 40 hours, the participants experienced three balanced crossover segments, each with a different light condition: dim light (DL: 8 lux, 2800 K), white light (WL: 250 lux, 2800 K), and blue-enriched white light (BL: 250 lux, 9000 K). This study used the KSS, actigraphy, and blood sampling for melatonin measurements to assess sleep, alertness, and circadian rhythm. The results showed that both WL and BL improved alertness and sleep quality in both age groups, but an evening rise in blood melatonin levels was only observed in young subjects under WL and BL.
An experimental randomized controlled trial was conducted utilizing identical light interventions and sustained wakefulness duration [64]. Slow wave activity/sleep (SWA, SWS), polysomnography, EEG recordings, and KSSCLE (Karolinska Sleepiness Scale, Core Level Effort) were employed. Researchers found similar results regarding the improvement in homeostatic sleep response after WL and BL compared to DL but no impact on SWS and SWA. Another lab-based study compared two hours of exposure to blue-enriched polychromatic light (6,500 K) and non-blue-enriched light (3,000 K or 2,500 K) at low levels of 40 lux in the evening on two groups of young and older adults in an observational counter- balanced within-subject crossover design study [67]. The KSS, Frontal slow-wave activity (SWA) by EEG and saliva sampling were used for assessments. The findings indicated reduced light sensitivity in older adults compared to younger adults, with implications for sleep and circadian rhythms in older adults. Improved alertness and sleep quality were observed in young subjects, but not in older adults.
In a balanced crossover study conducted by [66], the influence of 30 minutes exposure to light at night on 23 healthy older adults was studied through two overnight stays in the lab separated by one week. Participants were asked to sleep in complete darkness except for the last 30 minutes before wake-up time for one of the nights, during which a dawn simulation lighting condition ranging 0 to 250 lux was used to examine its impact on older adults’ alertness, circadian rhythm, and sleep quality. The results indicated that dawn simulation lighting increases the likelihood of waking at the end of the sleep period and improves overall sleep quality among the older population measured by actigraphy, PSG and SSS. However, no significant influence was found on alertness.
There are also studies that only considered objective measurements for sleep without considering subjective techniques and found significant results. This includes a randomized, placebo-controlled, mixed-study design by [62], which involved 17 older adults being exposed to two hours of morning typical light exposure of 500–1000 lux as a control group for five consecutive days. They then underwent two light conditions of 3000–5000 lux and 500–1000 lux as lighting intervention conditions. Actigraphy was the only used method and results indicated significant improvement of sleep initiation with morning bright light exposure. Another randomized lab experimental study utilized EEG for objective measurements and reported no changes in sleep duration or circadian timing in response to blue-enriched or blue-suppressed lighting conditions in older adults [7].
All in all, studies employing subjective techniques alone, such as questionnaires, generally found no significant impact of lighting on sleep quality and alertness in healthy older adults. However, studies combining objective measures, such as actigraphy and polysomnography, with subjective scales (e.g., SSS, KSS) consistently demonstrated the positive influence of appropriate lighting design. Interventions, such as blue-enriched white light and bright light exposure, improved both subjective and objective measures of sleep quality and alertness. These interventions also affected circadian rhythm, reduced sleepiness, and enhanced early evening sleep without compromising subsequent sleep. Therefore, this review reveals that to comprehensively understand lighting’s impact on sleep, a combination of objective and subjective assessment methods is recommended.
3.5.2. Field-based studies
Similar to lab-based studies, the results of the reviewed studies conducted in the field also showed that studies that employed both objective and subjective evaluation methods or only objective methods of assessments for sleep quality, alertness, and circadian rhythm had more significant results in comparison to the studies that only considered subjective surveys and questionnaires.
An experimental within-subject study conducted by [83] randomly assigned 14 older adults to different lighting conditions, including 80 to 100 lux with 2,700 K to 5,000 K as circadian lighting conditions for five weeks followed by 320 lux and 3500K as the placebo condition for another five weeks. This study employed PSQI as a subjective sleep quality assessment and found no significant differences between the two light conditions and no impact on sleep efficiency, sleep duration, or sleep latency. Another study [76] examined the relationship between illuminance and subjective sleep quality on a sample of 44 healthy older adults. This study concluded that living in environments without light and dark cycles could increase depression scores, but it did not find a significant correlation between lighting and subjective sleep quality measured by PSQI surveys. The authors suggested that the use of objective sleep measurements instead of subjective ones may explain the lack of significance in the effects of lighting conditions on sleep quality. Another observational before-after clinical trial study [77], asked older adults to be exposed to daylight for one hour in the morning (9:00–10:00 a.m.) and one hour in the evening (4:00–5:00 p.m.) and used KSS for sleep quality assessments. This study concluded that daylight exposure could result in delayed sleep phase and correction of circadian rhythm in older adults.
Studies that employed objective assessment methods or a combination of objective and subjective techniques revealed more significant results. For example, [82] conducted a quasi-experimental design study with pre-test and post-test measures in the field aimed at investigating the influence of 90 minutes of bright light exposure (7,000–10,000 lux) for five days a week, for three consecutive weeks, on 37 older adults. The QSQ and actigraphy were used for subjective and objective sleep and alertness measurements, respectively. The study showed a considerable improvement in circadian rhythm, sleep, and health outcomes. Another study by [37] also applied two whole-day ambient lighting interventions with high illuminance of 500 lux in the morning, gradually diminished to 100 lux in the evening. One of the lighting conditions had a constant CCT of 2,700 K, while the other had an altered CCT from 5,600 K to 2,700 K throughout the day. The results indicated that bright light in the morning significantly improved sleep, and having a gradually dimming lighting illuminance with decreasing CCT level was more effective in reducing sleep disturbance and sleep onset latency.
A field study [57] compared the percentage of waking time spent at four different light levels (ranging from 100 lux to 1000 lux) in older and younger adults, using actigraphy and sleep surveys. The results indicated that healthy older adults were exposed to higher levels of illuminance compared to younger individuals, and that natural light exposure may impact sleep-wake cycles. Obayashi and colleagues conducted a series of observational studies in field settings, examining the influence of light on circadian rhythm and sleep quality in older adults [71,73,87]. In one of their studies [71], melatonin levels were measured through blood sampling and actigraphy was used to assess sleep efficiency. The findings revealed a positive relationship between increased daylight exposure and better sleep quality in older adults. The authors continued their research in this field, and two years later assessed the effects of night light exposure on sleep quality in a sample of 875 older adults, using actigraphy, urinary tests for melatonin levels, and the PSQI surveys [87]. The results showed that exposure to high illuminance lighting at night was associated with diminished sleep quality. In another field study, researchers investigated the relationship between sleep onset latency and evening light exposure, using wrist-worn light trackers and actiwatches to objectively measure light exposure and sleep onset latency, respectively [73]. They found that evening light exposure significantly prolonged sleep onset latency and decreased sleep efficiency in older adults.
A few studies have investigated seasonal differences in the relationship between lighting conditions, alertness, and sleep in older adults. Researchers in [75] conducted a study to assess how seasonal variations in natural light exposure impact the sleep quality of older adults residing in nursing homes. The study utilized actigraphy, SAQ and ESS. The results revealed that higher natural light exposure during the summer months was associated with better sleep quality and increased alertness in older adults. It was also found that increasing the lighting illuminance at night weakened the sleep quality through bed-time delays and earlier wake-up times the next morning.
Similar to what have been found in lab-based studies, the reviewed field-based studies also show that employing a combination of objective and subjective assessment methods is crucial for assessing sleep effectively. Studies utilizing objective measures, such as actigraphy, melatonin sampling, and EEG, along with subjective measures, such as sleep questionnaires, have yielded significant results. Our review found only one study using mixed methods to evaluate sleep and alertness, with no significant findings on sleep duration and efficiency [74]. Additionally, we discovered only one study that relied solely on subjective evaluation via KSS, which yielded significant outcomes [77]. It is worth noting that field-based studies often involve longer durations of light exposure for participants, addressing one of the limitations observed in lab-based studies where shorter durations were applied. However, the implementation of certain objective assessment techniques, such as EEG for sleep evaluation, poses significant challenges in field settings. Additionally, requiring participants to use devices, such as actiwatches, for extended periods of time can be troublesome, adding to the complexity of conducting field-based studies in this field.
All in all, the discussed studies above predominantly assessed the initiation and quality of sleep, as well as the circadian rhythm and sleep phase in response to various lighting conditions. Morning bright light exposure consistently improved sleep initiation, while evening dimmed light exposures caused earlier evening sleepiness for older adults. Bright light therapy in the morning and high illuminance daylight exposure were beneficial in improving sleep quality and efficiency. While morning light exposure and dynamic, circadian-aligned lighting appear to be more effective in enhancing sleep quality and efficiency, increased light levels before bedtime and evening light exposure may adversely affect sleep initiation and efficiency.
3.6. Lighting, and cognitive performance
Among the 33 studies, 17 evaluated various domains of cognitive performance using different tests and methods. Seven studies assessed general cognitive functioning, primarily employing the Mini-Mental State Examination (MMSE) to evaluate awareness of time and place, memory and recall abilities, attention and concentration, language skills, and visual tasks. Beyond these, some studies specifically focused on particular cognitive domains rather than general cognitive functions. For instance, four studies examined visual tasks, predominantly using the Digit Symbol Substitution Test (DSST); three studies explored memory and concentration, mainly through test batteries; and seven studies investigated attention, with the Psychomotor Vigilance Task (PVT) being the most commonly used method. Table 5 provides a summary of the most common methods used in the studies to assess various domains of cognitive performance.
These studies are divided in two categories of laboratory-based and field-based studies which are explained in detail in the following sections.
3.6.1. Lab-based studies
Eight out of all reviewed studies were conducted in the lab environment and six of the studies concluded that there was a beneficial influence of lighting on various aspects of cognitive performance, including concentration and attention, working memory and memory capacity, and reaction time among healthy older adults.
In an experimental randomized controlled trial, the influence of bright light at night on cognitive performance and selected and divided attention was investigated on 32 healthy older adults [57]. Participants were exposed to bright light of 3000 lux from 10 p.m. to 2 a.m. for three consecutive nights in a lab visit. The rest of the night was spent in a room illumination of 300 lux. The results of the Attention test battery (Go/No-Go test) showed that while exposure to bright light at night reduced error rates for divided attention tasks, selective attention was not affected. In a similar study in terms of lighting condition and study design [58], working memory was evaluated by the level three test battery for attentional performance, concentration was examined by Konzentrations-Leistungs Test (KLT-R) and divided attention was evaluated by a subtest of the Attention Test Battery. The findings of the study indicated a strong correlation between bright light exposure at night and improvements in cognitive performance, particularly in working memory and concentration. In another randomized controlled trial [7], a comparison was made between blue-enriched polychromatic white (BEL) and polychromatic white light (WL) conditions in 10 healthy older adults. Working memory was assessed using the DSST. The results showed that exposure to blue-enriched white light in the evening had a greater impact on DSST performance the following morning compared to polychromatic white light.
Some studies also highlighted the significance of morning bright light and its positive impacts on cognitive performance in the laboratory environment. In a randomized, placebo-controlled, mixed-study design [62], the control group received two hours of morning typical light exposure ranging from 500 to 1,000 lux. The lighting intervention conditions included two groups: one exposed to 3000-5000 lux and the other to 500-1,000 lux, both from 9:00 a.m. to 11:00 a.m. This study used Digitized neuro psychological test battery for cognitive performance assessments and reported the importance of morning bright light exposure to overall cognitive ability scores and improved memory capacity. In another experimental within-subject study [64], 15 different lighting conditions, ranging from 300 to 1,500 lux and 3,000 to 6,500 K, were applied to 16 older adults to examine their influence on visual and cognitive performance. The results showed that increasing the CCT improved task performance, while lighting intensity had little impact. The authors concluded that short-duration light exposure may affect visual performance but has minimal influence on the physiological rhythm of the older adults.
This literature review reveals two contradictory studies that reported no influence on the working memory, attention, or cognitive performance of older adults as a result of being exposed to various lighting conditions. One within-subject study [60] investigated the effects of different lighting conditions, ranging from 300 lux to 2700 lux, on two groups of young and older adults. Cognitive performance was assessed using test-battery—including visual acuity, auditory PVT, and complex cognitive tasks involving executive function (Go/NoGo, Stroop, typing). The study found no statistically significant effects of light on these cognitive measures. Researchers of [66] also found no impact of dawn simulation lighting applied the last 30 minutes before the wake-up time of older adults on cognitive performance by using the Auditory version of the PVT.
In conclusion, the reviewed studies present conflicting results regarding the impact of lighting conditions on cognitive performance among older adults in lab-based settings. It seems there is no consistency in the recommended lighting conditions—either a bright light at night or a morning bright light exposure—to improve attention, cognitive ability scores, and memory capacity. These conflicting results indicate the need for further research to better understand the relationship between lighting and cognitive performance in lab-based settings.
3.6.2. Field-based studies
Eight of the studies were conducted in the field and six of them concluded that there was a beneficial influence of lighting on cognitive performance among older adults. Five of these studies were experimental and three of the studies observed the baseline lighting conditions along with the probable correlations among lighting and cognition.
Researcher in [70] conducted a study where participants were exposed to bright blue light of 400 lux for 30 minutes per day for four weeks, compared to a placebo red light of 75 lux. The researchers used the MicroCog Assessment of Cognitive Functioning, and Geriatric Depression Scale, and found that morning bright blue light had a significant impact on cognitive performance. Another study evaluated cognitive performance in older adults using Trail-Making Tests (TMT-A and TMT-B), DSST, Geriatric Depression Scale (GDS), and Positive and Negative Affect Schedule (PANAS) [31]. Their findings revealed that a lighting scheme with higher intensity and blue-enriched light with higher CCT in the morning and lower intensity with yellowish low CCT at night can improve cognitive performance in older adults. Results of [82] also indicate the beneficial impacts of morning bright light on improving cognitive performance assessed by MMSE Spanish validation.
Three observational studies [77–79] discovered positive correlations between exposure to daylight and cognitive performance in older adults. The evaluation methods employed were the VAS for study [77] and the MMSE for the two other mentioned studies.
Two studies didn’t find a significant impact of changing the intensity and color temperature of light on cognitive performance [80,83]. The former was a within-subject study conducted in which participants were randomly assigned to different lighting conditions and cognitive performance was evaluated by using various cognitive batteries tests, including Pattern Comparison and Processing Speed Test, Flanker Inhibitory Control, Attention Test, and Dimensional Change Card Sort Test. The latter used PVT and MMSE for cognition assessments and revealed that although blue-enriched lighting reduces anxiety, it has no significant impact on cognitive performance among older adults.
In conclusion, several methods have been identified as effective in assessing cognitive performance in field-based studies. The use of assessment tools, such as the MicroCog Assessment of Cognitive Functioning, TMT-A and TMT-B, DSST, GDS, and MMSE, has provided valuable insights into the relationship between lighting and cognitive performance among older adults. Experimental studies have shown that exposure to bright blue light in the morning can significantly improve cognitive performance, while observational studies have demonstrated positive correlations between exposure to daylight and cognitive performance. However, not all studies have found significant impacts, as some have reported no significant changes in cognitive performance when manipulating lighting conditions. Another critical finding from this review is the lack of evaluation on how light indirectly affects cognitive functions via improvements in sleep quality, an area crucial for future research.
The current body of research presents encouraging evidence regarding the beneficial impact of lighting exposure on enhancing the sleep quality and cognitive performance of healthy older adults. Optimal lighting conditions, particularly bright light with higher CCT and LUX values in the morning are poised to enhance sleep quality by improving sleep initiation, efficiency, and by minimizing sleep disturbances and latency. They also play a role in regulating the circadian rhythm and adjusting sleep phases. In terms of cognitive effects, lighting is particularly influential on working memory, concentration, and aspects of attention. However, the current literature lacks a comprehensive exploration of how lighting influences cognitive functions indirectly through its impact on sleep.
This field of study is marked by a considerable variation in lighting intervention methods, study designs, and participant demographics. This diversity complicates the process of drawing solid conclusions. As we delve deeper, we encounter a range of potential factors that could influence the findings, contributing to their inconsistency. It is important to note that these inconsistent outcomes should not be interpreted as a lack of effectiveness of lighting exposure. Instead, they more likely reflect the varied nature of the research conducted in this area.
Other review studies in this field have provided valuable insights aligned with this study's findings [15,34,88], yet none specifically focus on the methodologies, study setting and designs, evaluation methods and techniques, and characteristics of administered lighting conditions affecting sleep and cognitive performance. Moreover, they do not address the specific effects of lighting exposure on sleep and cognitive factors or discuss the broader non-visual impacts of light on human health [27, 89, 90]. While some reviews offer significant insights, they do not concentrate on the demographic of healthy older adults [18,91–93]. To date, there has been a notable absence of thorough reviews that explore these methodological aspects, study designs, lighting conditions, and evaluation tools, and how these aspects influence study outcomes, particularly on healthy older adults’ population.
We discussed our findings in the following paragraphs in more detail.
4.1. Study setting and design
The review included both lab-based and field measurement studies, and the results indicate that most of the experimental studies were conducted in the lab environment, whereas a large number of the field studies were based on observations of the participants’ baseline lighting exposure, without applying lighting intervention.
Conducted experimental lab-based studies found significant results, although they lack the ability to investigate the impact of lighting design in real-world settings. There is a need for further experimental field-based studies that are more representative of the everyday environment of older adults. Also, older adults may find it more difficult to adhere to a strict lab-based study protocol, and studying the influence of lighting in their natural living condition seems to provide more naturalistic results. Studies that apply participants randomly to different lighting conditions and have control over the order of lighting treatments being given to different individuals result in more significant outcomes. Moreover, the findings indicate that studies employing a combination of within-subject and between-subject designs with a crossover approach provide better control over variables and yield more reliable results compared to between-subject studies where participants are randomly assigned to only one of the experimental lighting conditions. A crossover study offers the advantage of minimizing potential confounding personality variables by using each participant as their own control. This approach effectively decreases variability, resulting in an enhanced statistical power [58].
The majority of the studies involved participants who exhibited good physical and psychological health, normal visual acuity, and no previous record of substance abuse or medication usage that could potentially influence sleep and cognition. However, there is an important gap in the inclusion criteria of the studies regarding the record of daily light exposure of the selected participants, which has been only considered in one of the reviewed studies [87]. This is an important inclusion criterion as being outside and exposed to daylight even for a few hours has a light entrainment effect that last several hours [94] and may affect the results. Other study limitations include small sample sizes, limited participant demographic diversity, including race, and study location, which constrain the findings' generalizability. Moreover, there's a notable lack of reporting on statistical test assumptions and effect sizes. Determination and justification of sample sizes, reporting effect sizes and test assumptions are crucial to reduce errors and enhance the validity of the results [95].
4.2. Lighting condition and implementation in practice settings
Initially, white light sources were commonly used as a light therapy method, but studies later revealed the impact of short-wavelength light on melatonin suppression and circadian rhythm in humans. Some of the studies only considered the light intensity by assessing the impact of bright light in comparison to a dimmed light condition.
The application of bright light with higher lux and CCT values at various times from early morning to early evening has been shown to yield beneficial effects on sleep and cognitive functions, particularly working memory and concentration domains, though the optimal timing for such treatments remains elusive. However, complications arise with the use of light featuring high amounts of short wavelengths and the deployment of overly intense placebo lights, which have sometimes negated the benefits of bright light. These issues underscore the necessity for meticulous consideration in choosing placebo conditions, as even moderate levels of light can substantially influence sleep patterns, circadian rhythms, and cognitive functions. Although some studies highlight the benefits of using bright light at night or late evening to enhance cognitive functions and reduce error rates among older adults, this review reveals that this practice can negatively impact sleep quality. Furthermore, the mediated effects of disrupted sleep must be considered, as they could indirectly compromise cognitive functions.
This review found that studies that considered both light intensity and correlated color temperature of light found more promising and significant results. The reviewed studies present a lack of consistency in applied lighting conditions. The studies also used different values considered as bright light, placebo, blue-enriched, and blue-suppressed lighting conditions in terms of lux level and CCT [31,70,74,82,84], which further complicate the interpretation of the results. Melatonin levels are suppressed during the day as light enters the eye and the spectral response of this process peaks at blue light of around 470-480 nm [32]. While a previous lab-based study conducted by [82] mentioned that melatonin levels are increased by eye illuminance as low as 50 lux, this review shows that several studies reported improvements in sleep and cognition for test subjects being exposed to higher amount of light during the study [31,37,64]. Only a limited number of studies provided information regarding the Spectral Power Distribution (SPD) of the interventional lighting conditions implemented in their experiments [31,37,61,74]. This shows a significant limitation within these studies, as CCT alone does not sufficiently capture the complexity of SPD, which is a crucial factor in understanding the circadian effects of light. While a number of studies provided detailed descriptions of lighting interventions, specifying measurement directions (e.g., vertically at the participants' eye level) and quantifying circadian lighting variables such as Equivalent Melanopic Lux (EML), Minimum Melanopic EDI (MEDI), and Circadian Stimulus (CS) [31,37,64], the vast majority did not offer comprehensive details on the lighting interventions. Thus, it is imperative to consider all lighting factors when investigating the impact of lighting on circadian rhythms, ensuring a comprehensive assessment of the light’s characteristics and their potential physiological implications. Furthermore, many studies neglected to provide detailed information on measurement direction (e.g., vertically at the participants' eye level). Another notable research gap identified in the reviewed studies is the insufficient information regarding the specifics of the implemented lighting interventions, particularly the types of luminaires used. This detail is of significant importance [80] yet often overlooked in the documentation of these studies.
Light exposure duration is another factor that should be considered in the studies. Short duration of light exposure cannot show the optimal impact of lighting and may result in insignificant research findings.
Partly, this can be attributed to the absence of a robust theoretical model that guides research in this field as study duration varies between a few minutes of light exposure [61] to several weeks and months [74,77,83]. For accurate assessment of light exposure, it's essential to measure light levels at eye level, rather than using indirect methods like wrist-level actigraphs [81]. Another limitation is the imprecise tracking of participants' exposure time to light interventions, particularly in field studies as well as the amount of time participants spend outdoors during the day and therefore different daylight exposure, which is an important factor affecting sleep and cognition. The adoption of objective measurement tools, like light trackers, could offer more control and accuracy in quantifying this exposure. Additionally, it's important to ensure that lighting is not only effective but also comfortable and aesthetically pleasing, maintaining levels that are both acceptable and conducive to well-being.
4.3. Methods of assessment
The assessment of sleep quality and cognitive performance in older adults has evolved in fresearch studies, with changes in methodologies and tools over time. The studies reviewed used various surveys, questionnaires, and objective or subjective measurement techniques to assess sleep, alertness, and cognitive performance. The results of this review revealed that studies that only considered subjective evaluations, such as surveys and questionnaires, did not find significant results, and studies that employed both objective and subjective techniques found more promising findings [37,56,82]. Some studies had limitations, such as a lower number of participants who accept to enroll in objective, measurements, such as actigraphy or saliva and blood sampling for evaluating sleep and melatonin levels, and therefore obtained subjective questionnaires for their evaluations. Also, regarding the objective methods, polysomnography and EEG are more feasible in the lab environment and not in the natural settings of the field, such as residential units of the older adults, and actigraphy has been used as the most common technique that revealed significant results to assess sleep objectively in the field. Studies that employed frontal slow wave activity by EEG and Digitized neuro psychological test battery, Micro Cog Assessment of Cognitive Functioning, MMSE, PVT, DSST, and test batteries for cognition, working memory, and selective and divided attention draw more significant results [7,31,58,62].
5. Conclusions and recommendations for future studies
To summarize, this review underscores the necessity for further research to establish a correlation between lighting conditions and the sleep quality, and cognitive performance of healthy older adults. The aforementioned findings are derived from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. It exclusively encompasses studies focused on healthy older adults, aiming to find research gaps in methodology and lighting design solutions for mitigating the risk of Alzheimer’s and dementia. Future research should meticulously evaluate various aspects of lighting, including spectral power distribution (SPD), correlated color temperature (CCT), intensity, and duration of exposure and quantify circadian lighting variables, including EML, MEDI, or CS values. This will enable a more precise and comprehensive understanding of how lighting impacts sleep and cognitive functions in this demographic. Bright light, applied from early morning to early evening, has shown to improve sleep and cognitive functions, especially working memory and concentration, though the best timing remains unclear. However, complications like the use of intense short-wavelength lights and intense placebo conditions can negate these benefits, and evening applications may disrupt sleep and indirectly affect cognitive performance in older adults. Notably, the dominance of lab-based studies in this field calls for an increased focus on field-based experimental studies that blend both objective and subjective methods for more solid outcomes. Well-designed Randomized Controlled Trials (RCTs) are essential to advance our understanding of light interventions. Future studies must be carefully planned to control for potential confounding variables and individual differences, ensuring standardized and balanced light exposure conditions. Implementing blinded studies can significantly reduce biases, whether from researchers or participants. Moreover, addressing issues such as small sample sizes, statistical test assumptions, and reporting of effect sizes can significantly enhance the quality and evidential value of lighting research. All in all, the inconsistent results in lighting studies should not be considered as a lack of effectiveness. Rather, they likely indicate the diverse approaches and methodologies used in this research area and It's crucial to employ rigorous study designs and thorough assessment methods to accurately determine the optimal lighting treatment approach for this population.
Contributions
Mahya Fani: Writing–original draft, Investigation and comprehensive literature review, Project administration Methodology, Conceptualization, Visualization. Nina Sharp: Writing – review & editing, Supervision, Project administration, Methodology, Conceptualization.
Acknowledgment
We gratefully acknowledge the contributions of all individuals who assisted in the development of this manuscript. We also extend our appreciation to the reviewers for their valuable feedback.
Declaration of competing interest
The authors declare no conflict of interest.
References
- J. Reijnders, C. van Heugten, M. van Boxtel, Cognitive interventions in healthy older adults and people with mild cognitive impairment: A systematic review, Ageing Res. Rev. 12 (2013) 263-275. https://doi.org/10.1016/j.arr.2012.07.003
- I. Konstantzos, S.A. Sadeghi, M. Kim, J. Xiong, A. Tzempelikos, The effect of lighting environment on task performance in buildings - A review, Energy Build. 226 (2020). https://doi.org/10.1016/j.enbuild.2020.110394
- A. Tsapanou, Y. Gu, D.M. O'Shea, M. Yannakoulia, M. Kosmidis, E. Dardiotis, G. Hadjigeorgiou, P. Sakka, Y. Stern, N. Scarmeas, Sleep quality and duration in relation to memory in the elderly: Initial results from the Hellenic Longitudinal Investigation of Aging and Diet, Neurobiol. Learn. Mem. 141 (2017) 217-225. https://doi.org/10.1016/j.nlm.2017.04.011
- J.H. Kim, J.H. Ahn, C.Y. Min, D.M. Yoo, H.G. Choi, Association between sleep quality and subjective cognitive decline: evidence from a community health survey, Sleep Med. 83 (2021) 123-131. https://doi.org/10.1016/j.sleep.2021.04.031
- C. Wang, F. Zhang, J. Wang, J.K. Doyle, P.A. Hancock, C.M. Mak, S. Liu, How indoor environmental quality affects occupants' cognitive functions: A systematic review, Build. Environ. 193 (2021). https://doi.org/10.1016/j.buildenv.2021.107647
- J. Potočnik, M. Košir, Influence of geometrical and optical building parameters on the circadian daylighting of an office, J. Build. Eng. 42 (2021). https://doi.org/10.1016/j.jobe.2021.102402
- K. Scheuermaier, M. Münch, J.M. Ronda, J.F. Duffy, Improved cognitive morning performance in healthy older adults following blue-enriched light exposure on the previous evening, Behav. Brain Res. 348 (2018) 267-275. https://doi.org/10.1016/j.bbr.2018.04.021
- Z. Wang, H. Yu, M. Luo, Z. Wang, H. Zhang, Y. Jiao, Predicting older people's thermal sensation in building environment through a machine learning approach: Modelling, interpretation, and application, Build. Environ. 161 (2019). https://doi.org/10.1016/j.buildenv.2019.106231
- M. Leung, C. Wang, T.C. Kwok, Effects of supporting facilities on memory loss among older people with dementia in care and attention homes, Indoor Built Environ. 29 (2020) 438-448. https://doi.org/10.1177/1420326X19886344
- M. Cricco, E.M. Simonsick, D.J. Foley, The Impact of Insomnia on Cognitive Functioning in Older Adults, J Am Geriatr Soc 49 (2001) 1185-1189. https://doi.org/10.1046/j.1532-5415.2001.49235.x
- M. Leng, H. Yin, P. Zhang, Y. Jia, M. Hu, G. Li, C. Wang, L. Chen, Sleep Quality and Health-Related Quality of Life in Older People With Subjective Cognitive Decline, Mild Cognitive Impairment, and Alzheimer Disease, J. Nerv. Ment. Dis. 208 (2020) 387-396. https://doi.org/10.1097/NMD.0000000000001137
- P. Siddarth, K. Thana-Udom, R. Ojha, D. Merrill, J.M. Dzierzewski, K. Miller, G.W. Small, L. Ercoli, Sleep quality, neurocognitive performance, and memory self-appraisal in middle-aged and older adults with memory complaints, Int. Psychogeriatr. 33 (2021) 703-713. https://doi.org/10.1017/S1041610220003324
- L. Pini, A. Wennberg, M. Mitolo, F. Meneghello, F. Burgio, C. Semenza, A. Venneri, D. Mantini, A. Vallesi, Quality of sleep predicts increased frontoparietal network connectivity in patients with mild cognitive impairment, Neurobiol. Aging 95 (2020) 205-213. https://doi.org/10.1016/j.neurobiolaging.2020.07.026
- I. Jaussent, J. Bouyer, M.L. Ancelin, C. Berr, A. Foubert-Samier, K. Ritchie, M.M. Ohayon, A. Besset, Y. Dauvilliers, Excessive sleepiness is predictive of cognitive decline in the elderly, Sleep 35 (2012) 1201-1207. https://doi.org/10.5665/sleep.2070
- P. Nylén, F. Favero, S. Glimne, K. Teär Fahnehjelm, J. Eklund, Vision, light and aging: A literature overview on older-age workers, Work 47 (2014) 399-412. https://doi.org/10.3233/WOR-141832
- S. Kumar, S.H. Underwood, J.L. Masters, N.A. Manley, I. Konstantzos, J. Lau, R. Haller, L.M. Wang, Ten questions concerning smart and healthy built environments for older adults, Build. Environ. 244 (2023) 110720. https://doi.org/10.1016/j.buildenv.2023.110720
- World Health Organization (WHO). Constitution of the World Health Organization, (1948).
- G.J. Hjetland, S. Pallesen, E. Thun, E. Kolberg, I.H. Nordhus, E. Flo, Light interventions and sleep, circadian, behavioral, and psychological disturbances in dementia: A systematic review of methods and outcomes, Sleep Med. Rev. 52 (2020) 101310. https://doi.org/10.1016/j.smrv.2020.101310
- S. Ancoli-Israel, P. Gehrman, J.L. Martin, T. Shochat, M. Marler, J. Corey-Bloom, L. Levi, Increased Light Exposure Consolidates Sleep and Strengthens Circadian Rhythms in Severe Alzheimer's Disease Patients, Behav. Sleep. Med. 1 (2003) 22-36. https://doi.org/10.1207/S15402010BSM0101_4
- D. Forbes, C.M. Blake, E.J. Thiessen, S. Peacock, P. Hawranik, Light therapy for improving cognition, activities of daily living, sleep, challenging behaviour, and psychiatric disturbances in dementia, Cochrane Database Syst. Rev. (2014). https://doi.org/10.1002/14651858.CD003946.pub4
- W.J.M. van Bommel, G.J. van den Beld, Lighting for work: A review of visual and biological effects, Light. Res. Technol. 36 (2004) 255-269. https://doi.org/10.1191/1365782804li122oa
- P.R. Boyce, Review: The Impact of Light in Buildings on Human Health, Indoor Built Environ. 19 (2010) 8-20. https://doi.org/10.1177/1420326X09358028
- R. Sithravel, R. Ibrahim, Identifying supportive daytime lighting characteristics for enhancing individuals' psychophysiological wellbeing in windowless workplace in tropical Malaysia, Indoor Built Environ. 30 (2021) 298-312. https://doi.org/10.1177/1420326X19889656
- J. Van Duijnhoven, M.P.J. Aarts, M.B.C. Aries, A.L.P. Rosemann, H.S.M. Kort, Systematic review on the interaction between office light conditions and occupational health: Elucidating gaps and methodological issues, Indoor Built Environ. 28 (2019) 152-174. https://doi.org/10.1177/1420326X17735162
- L. Edwards, P. Torcellini, A Literature Review of the Effects of Natural Light on Building Occupants, 2002. http://www.osti.gov/bridge.
- J.F. Duffy, K.P. Wright, Entrainment of the Human Circadian System by Light, J. Biol. Rhythms 20 (2005) 326-338. https://doi.org/10.1177/0748730405277983
- O. Osibona, B.D. Solomon, D. Fecht, Lighting in the home and health: A systematic review, Int. J. Environ. Res. Public. Health 18 (2021) 1-20. https://doi.org/10.3390/ijerph18020609
- C.B. Swope, S. Rong, C. Campanella, R. Vaicekonyte, A.J. Phillips, S.W. Cain, E.M. McGlashan, Factors associated with variability in the melatonin suppression response to light: A narrative review, Chronobiol. Int. 40 (2023) 542-556. https://doi.org/10.1080/07420528.2023.2188091
- L.H.S. De Toledo, M.N. Moraes, M.D.O. Poletini, J.C. Neto, J. Baron, T. Mota, Modeling the influence of nighttime light on melatonin suppression in humans: Milestones and perspectives, J. Photochem. Photobiol. 16 (2023) 100199. https://doi.org/10.1016/j.jpap.2023.100199
- C. Cajochen, Alerting effects of light, Sleep Med. Rev. 11 (2007) 453-464. https://doi.org/10.1016/j.smrv.2007.07.009
- N. Shishegar, M. Boubekri, Lighting up living spaces to improve mood and cognitive performance in older adults, J. Environ. Psychol. 82 (2022). https://doi.org/10.1016/j.jenvp.2022.101845
- I Provencio, H.M. Cooper, R.G. Foster, ; J Hannibal, Phototransduction by Retinal Ganglion Cells That Set the Circadian Clock, 1998. www.sciencemag.org.
- M. Anaraki, M. Fani, A.F. Shahverdi, Z.S. Zomorodian, Evaluation of the effects of partition design on circadian daylighting in open-plan offices, Sol. Energy 264 (2023) 112067. https://doi.org/10.1016/j.solener.2023.112067
- S. Shikder, M. Mourshed, A. Price, Therapeutic lighting design for the elderly: A review, Perspect. Public Health 132 (2012) 282-291. https://doi.org/10.1177/1757913911422288
- D. L. Sturnieks, R. St George, S. R. Lord, Balance disorders in the elderly, Neurophysiol. Clin. 38 (2008) 467-478. https://doi.org/10.1016/j.neucli.2008.09.001
- C. Owsley, Vision and Aging, Annu. Rev. Vis. Sci. 2 (2016) 255-271. https://doi.org/10.1146/annurev-vision-111815-114550. https://doi.org/10.1146/annurev-vision-111815-114550
- N. Shishegar, M. Boubekri, E.A.L. Stine-Morrow, W.A. Rogers, Tuning environmental lighting improves objective and subjective sleep quality in older adults, Build. Environ. 204 (2021). https://doi.org/10.1016/j.buildenv.2021.108096
- P. Khademagha, M.B.C. Aries, A.L.P. Rosemann, E.J. van Loenen, Implementing non-image-forming effects of light in the built environment: A review on what we need, Build. Environ. 108 (2016) 263-272. https://doi.org/10.1016/j.buildenv.2016.08.035
- I. Campbell, R. Sharifpour, G. Vandewalle, Light as a Modulator of Non-Image-Forming Brain Functions-Positive and Negative Impacts of Increasing Light Availability, Clocks Sleep 5 (2023) 116-140. https://doi.org/10.3390/clockssleep5010012
- M.L. Amundadottir, S. Rockcastle, M. Sarey Khanie, M. Andersen, A human-centric approach to assess daylight in buildings for non-visual health potential, visual interest and gaze behavior, Build. Environ. 113 (2017) 5-21. https://doi.org/10.1016/j.buildenv.2016.09.033
- J. Potočnik, M. Košir, M. Dovjak, Colour preference in relation to personal determinants and implications for indoor circadian luminous environment, Indoor Built Environ. 31 (2022) 121-138. https://doi.org/10.1177/1420326X20977609
- M. Fani, N. Sharp, M. Anaraki, A.F. Shahverdi, Evaluation of the influence of interior design parameters on circadian daylighting of design-studio classrooms, in: 2023. https://doi.org/10.26868/25222708.2023.1323
- G.C. Brainard, D. Sliney, J.P. Hanifin, G. Glickman, B. Byrne, J.M. Greeson, S. Jasser, E. Gerner, M.D. Rollag, Sensitivity of the human circadian system to short-wavelength (420-nm) light, J. Biol. Rhythms 23 (2008) 379-386. https://doi.org/10.1177/0748730408323089
- M.G. Figueiro, E. Saldo, M.S. Rea, K. Kubarek, J. Cunningham, M.S. Rea, Developing Architectural Lighting Designs to Improve Sleep in Older Adults, 2008. https://doi.org/10.2174/1874620900801010040
- E. van Lieshout-van Dal, L. Snaphaan, I. Bongers, Biodynamic lighting effects on the sleep pattern of people with dementia, Build. Environ. 150 (2019) 245-253. https://doi.org/10.1016/j.buildenv.2019.01.010
- C.A. Alessi, J.L. Martin, A.P. Webber, E.C. Kim, J.O. Harker, K.R. Josephson, Randomized, controlled trial of a nonpharmacological intervention to improve abnormal sleep/wake patterns in nursing home residents, J. Am. Geriatr. Soc. 53 (2005) 803-810. https://doi.org/10.1111/j.1532-5415.2005.53251.x
- S. Ancoli-Israel, Sleep disorders in the elderly, 2010. https://www.researchgate.net/publication/42389740.
- N. Hanford, M. Figueiro, Light therapy and Alzheimer's disease and related dementia: Past, present, and future, J. Alzheimers Dis. 33 (2013) 913-922. https://doi.org/10.3233/JAD-2012-121645
- K. Konis, Field evaluation of the circadian stimulus potential of daylit and non-daylit spaces in dementia care facilities, Build. Environ. 135 (2018) 112-123. https://doi.org/10.1016/j.buildenv.2018.03.007
- M. Figueiro, B. Plitnick, A. Lok, G. Jones, P. Higgins, T. Hornick, M. Rea, Tailored lighting intervention improves measures of sleep, depression, and agitation in persons with Alzheimer’s disease and related dementia living in long-term care facilities, Clin. Interv. Aging (2014) 1527. https://doi.org/10.2147/CIA.S68557
- A. Skjerve, F. Holsten, D. Aarsland, B. Bjorvatn, H.A. Nygaard, I.M. Johansen, Improvement in behavioral symptoms and advance of activity acrophase after short‐term bright light treatment in severe dementia, Psychiatry Clin. Neurosci. 58 (2004) 343-347. https://doi.org/10.1111/j.1440-1819.2004.01265.x
- Y.-L. Jao, J. Wang, Y.-J. Liao, J. Parajuli, D. Berish, M. Boltz, K. Van Haitsma, N. Wang, L. McNally, M. Calkins, Effect of Ambient Bright Light on Behavioral and Psychological Symptoms in People With Dementia: A Systematic Review, Innov. Aging 6 (2022) igac018. https://doi.org/10.1093/geroni/igac018
- G. Marquardt, K. Bueter, T. Motzek, Impact of the Design of the Built Environment on People with Dementia: An Evidence-Based Review, HERD Health Environ. Res. Des. J. 8 (2014) 127-157. https://doi.org/10.1177/193758671400800111
- I. Goudriaan, L.C. Van Boekel, M.E. Verbiest, J. Van Hoof, K.G. Luijkx, Dementia Enlightened?! A Systematic Literature Review of the Influence of Indoor Environmental Light on the Health of Older Persons with Dementia in Long-Term Care Facilities, Clin. Interv. Aging Volume 16 (2021) 909-937. https://doi.org/10.2147/CIA.S297865
- M.J. Page, J.E. McKenzie, P.M. Bossuyt, I. Boutron, T.C. Hoffmann, C.D. Mulrow, L. Shamseer, J.M. Tetzlaff, E.A. Akl, S.E. Brennan, R. Chou, J. Glanville, J.M. Grimshaw, A. Hróbjartsson, M.M. Lalu, T. Li, E.W. Loder, E. Mayo-Wilson, S. McDonald, L.A. McGuinness, L.A. Stewart, J. Thomas, A.C. Tricco, V.A. Welch, P. Whiting, D. Moher, The PRISMA 2020 statement: An updated guideline for reporting systematic reviews, Int. J. Surg. 88 (2021). https://doi.org/10.1016/j.ijsu.2021.105906
- M. Münch, V. Bromundt, Light and chronobiology: Implications for health and disease, Dialogues Clin. Neurosci. 14 (2012) 448-453. https://doi.org/10.31887/DCNS.2012.14.4/mmuench
- V. Kretschmer, B. Griefahn, K.H. Schmidt, Bright light and night work: Effects on selective and divided attention in elderly persons, Light. Res. Technol. 43 (2011) 473-486. https://doi.org/10.1177/1477153511405808
- V. Kretschmer, K.H. Schmidt, B. Griefahn, Bright-light effects on cognitive performance in elderly persons working simulated night shifts: Psychological well-being as a mediator?, Int. Arch. Occup. Environ. Health 86 (2013) 901-914. https://doi.org/10.1007/s00420-012-0826-9
- T. Kim, S. Lim, S.G. Yoon, D. (Jason) Yeom, Pupil size and gender-driven occupant's productivity predictive model for diverse indoor lighting conditions in the office environment, Build. Environ. 226 (2022). https://doi.org/10.1016/j.buildenv.2022.109673
- P.M.C. Lemmens, L.J.M. Schlangen, A.J.M. Denissen, H.J. Talen, H.M.L. Herremans, D. Ruyter, Workplace illumination effects on acuity cognitive performance and well-being in older and young people, Proceedings of 28th CIE Session, 2015, 87.
- V. Gabel, C.F. Reichert, M. Maire, C. Schmidt, L.J.M. Schlangen, V. Kolodyazhniy, C. Garbazza, C. Cajochen, A.U. Viola, Differential impact in young and older individuals of blue-enriched white light on circadian physiology and alertness during sustained wakefulness, Sci. Rep. 7 (2017). https://doi.org/10.1038/s41598-017-07060-8
- Y. Dagan, G. Amit. Functional Consequences of Light Treatment in Healthy Older Adults Living in Residential Facility, Ann Sleep Med Res. 2018, 2 (1) 1010.
- K.D. Scheuermaier, J.H. Lee, J.F. Duffy, Phase Shifts to a Moderate Intensity Light Exposure in Older Adults: A Preliminary Report, J. Biol. Rhythms 34 (2019) 98-104. https://doi.org/10.1177/0748730418818655
- C. Cajochen, C. Reichert, M. Maire, L.J.M. Schlangen, C. Schmidt, A.U. Viola, V. Gabel, Evidence That Homeostatic Sleep Regulation Depends on Ambient Lighting Conditions during Wakefulness, Clocks Sleep 1 (2019) 517-531. https://doi.org/10.3390/clockssleep1040040
- Y. Wang, H. Huang, G. Chen, Effects of lighting on ECG, visual performance and psychology of the elderly, Optik 203 (2020). https://doi.org/10.1016/j.ijleo.2019.164063
- V. Gabel, M. Miglis, J.M. Zeitzer, Effect of artificial dawn light on cardiovascular function, alertness, and balance in middle-aged and older adults, Sleep 43 (2020). https://doi.org/10.1093/sleep/zsaa082
- S.L. Chellappa, V. Bromundt, S. Frey, C. Cajochen, Age-related neuroendocrine and alerting responses to light, GeroScience 43 (2021) 1767-1781. https://doi.org/10.1007/s11357-021-00333-1
- K. Missildine, N. Bergstrom, J. Meininger, K. Richards, M.D. Foreman, FEATURE ARTICLE Sleep in Hospitalized Elders: A Pilot Study, n.d. https://doi.org/10.1016/j.buildenv.2018.10.058
- K. Scheuermaier, A.M. Laffan, J.F. Duffy, Light exposure patterns in healthy older and young adults, J. Biol. Rhythms 25 (2010) 113-122. https://doi.org/10.1177/0748730410361916
- M. Royer, N.H. Ballentine, P.J. Eslinger, K. Houser, R. Mistrick, R. Behr, K. Rakos, Light therapy for seniors in long term care, J. Am. Med. Dir. Assoc. 13 (2012) 100-102. https://doi.org/10.1016/j.jamda.2011.05.006
- K. Obayashi, K. Saeki, J. Iwamoto, N. Okamoto, K. Tomioka, S. Nezu, Y. Ikada, N. Kurumatani, Positive effect of daylight exposure on nocturnal urinary melatonin excretion in the elderly: A cross-sectional analysis of the HEIJO-KYO study, J. Clin. Endocrinol. Metab. 97 (2012) 4166-4173. https://doi.org/10.1210/jc.2012-1873
- M.G. Figueiro, R. Hamner, P. Higgins, T. Hornick, M.S. Rea, Field measurements of light exposures and circadian disruption in two populations of older adults, J. Alzheimers Dis. 31 (2012) 711-715. https://doi.org/10.3233/JAD-2012-120484
- K. Obayashi, K. Saeki, N. Kurumatani, Association between light exposure at night and insomnia in the general elderly population: The HEIJO-KYO cohort, Chronobiol. Int. 31 (2014) 976-982. https://doi.org/10.3109/07420528.2014.937491
- B. Sander, J. Markvart, L. Kessel, A. Argyraki, K. Johnsen, Can sleep quality and wellbeing be improved by changing the indoor lighting in the homes of healthy, elderly citizens?, Chronobiol. Int. 32 (2015) 1049-1060. https://doi.org/10.3109/07420528.2015.1056304
- K. Tsuzuki, I. Mori, T. Sakoi, Y. Kurokawa, Effects of seasonal illumination and thermal environments on sleep in elderly men, Build. Environ. 88 (2015) 82-88. https://doi.org/10.1016/j.buildenv.2014.10.001
- A. Ichimori, K. Tsukasaki, E. Koyama, Illuminance, Subjective Sleep Quality, and Psychosomatic Health in Elderly Individuals Requiring Care: A Survey of Japan's Hokuriku Region in Winter, J. Community Health Nurs. 32 (2015) 104-114. https://doi.org/10.1080/07370016.2015.1026158
- Z. Karami, R. Golmohammadi, A. Heidaripahlavian, J. Poorolajal, R. Heidarimoghadam, Effect of Daylight on Melatonin and Subjective General Health Factors in Elderly People, Iranian journal of public health. 2016, 45(5) 636.
- A. Nioi, J. Roe, A. Gow, D. McNair, P. Aspinall, Seasonal Differences in Light Exposure and the Associations With Health and Well-Being in Older Adults: An Exploratory Study, Health Environ. Res. Des. J. 10 (2017) 64-79. https://doi.org/10.1177/1937586717697650
- J.A. Rubiño, A. Gamundí, M. Akaarir, F. Cañellas, R. Rial, N. Ballester, M.C. Nicolau, Effects of differences in the availability of light upon the circadian rhythms of institutionalized elderly, Chronobiol. Int. 34 (2017) 1197-1210. https://doi.org/10.1080/07420528.2017.1356840
- S. Hopkins, P.L. Morgan, L.J.M. Schlangen, P. Williams, D.J. Skene, B. Middleton, Blue-Enriched Lighting for Older People Living in Care Homes: Effect on Activity, Actigraphic Sleep, Mood and Alertness, Curr. Alzheimer Res. 14 (2017). https://doi.org/10.2174/1567205014666170608091119
- M. P. J. Aarts, J. C. Stapel, Toine A. M. C. Schoutens, Joost van Hoof, Exploring the Impact of Natural Light Exposure on Sleep of Healthy Older Adults: A Field Study, Journal of Daylighting 5 (2018) 5-14. https://doi.org/10.15627/jd.2018.2
- J.A. Rubiño, A. Gamundí, M. Akaarir, F. Canellas, R. Rial, M.C. Nicolau, Bright Light Therapy and Circadian Cycles in Institutionalized Elders, Front. Neurosci. 14 (2020). https://doi.org/10.3389/fnins.2020.00359
- M. Juda, T. Liu-Ambrose, F. Feldman, C. Suvagau, R.E. Mistlberger, Light in the Senior Home: Effects of Dynamic and Individual Light Exposure on Sleep, Cognition, and Well-Being, Clocks Sleep 2 (2020) 557-576. https://doi.org/10.3390/clockssleep2040040
- J.E. Elliott, C.E. Tinsley, C. Reynolds, R.J. Olson, K.B. Weymann, W.T.M. Au-Yeung, A. Wilkerson, J.A. Kaye, M.M. Lim, Tunable White Light for Elders (TWLITE): A Protocol Demonstrating Feasibility and Acceptability for Deployment, Remote Data Collection, and Analysis of a Home-Based Lighting Intervention in Older Adults, Sensors 22 (2022). https://doi.org/10.3390/s22145372
- S.J. Kim, S. Benloucif, K.J. Reid, S. Weintraub, N. Kennedy, L.F. Wolfe, P.C. Zee, Phase-shifting response to light in older adults, J. Physiol. 592 (2014) 189-202. https://doi.org/10.1113/jphysiol.2013.262899
- G. Eilertsen, G. Horgen, T.M. Kvikstad, H.K. Falkenberg, Happy Living in Darkness! Indoor Lighting in Relation to Activities of Daily Living, Visual and General Health in 75-Year-Olds Living at Home, J. Hous. Elder. 30 (2016) 199-213. https://doi.org/10.1080/02763893.2016.1162256
- K. Obayashi, K. Saeki, J. Iwamoto, N. Okamoto, K. Tomioka, S. Nezu, Y. Ikada, N. Kurumatani, Effect of exposure to evening light on sleep initiation in the elderly: A longitudinal analysis for repeated measurements in home settings, Chronobiol. Int. 31 (2014) 461-467. https://doi.org/10.3109/07420528.2013.840647
- X. Lu, N.K. Park, S. Ahrentzen, Lighting Effects on Older Adults' Visual and Nonvisual Performance: A Systematic Review, J. Hous. Elder. 33 (2019) 298-324. https://doi.org/10.1080/02763893.2018.1562407
- Department of Civil Engineering, Technische Universität Kaiserslautern, Germany, M. Alwalidi, S. Hoffmann, Department of Civil Engineering, Technische Universität Kaiserslautern, Germany, Alerting Effect of Light: A Review of Daytime Studies, J. Daylighting 9 (2022) 150-163. https://doi.org/10.15627/jd.2022.12
- M. Cheshmeh Noor, V. Revell, F. Mehdizadeh Saradj, S.-A. Yazdanfar, The impact of wavelength on acute non-visual responses to light: A systematic review and meta-analysis, Brain Res. 1816 (2023) 148470. https://doi.org/10.1016/j.brainres.2023.148470
- Y. Li, W. Fang, H. Qiu, W. Dong, J. Wang, H. Bao, Diurnal Intervention Effects of Electric Lighting on Alertness, Cognition, and Mood in Healthy Individuals: A Systematic Review and Meta-Analysis, LEUKOS (2023) 1-19. https://doi.org/10.1080/15502724.2023.2279946
- Y.-M. Mu, X.-D. Huang, S. Zhu, Z.-F. Hu, K.-F. So, C.-R. Ren, Q. Tao, Alerting effects of light in healthy individuals: a systematic review and meta-analysis, Neural Regen. Res. 17 (2022) 1929. https://doi.org/10.4103/1673-5374.335141
- M.C. Noor, F.M. Saradj, S.-A. Yazdanfar, Analytical evolution of measurement methods for light's non-visual effects, Results Eng. 17 (2023) 100922. https://doi.org/10.1016/j.rineng.2023.100922
- Reinhart, C. Daylighting Handbook I: Fundamentals [and] Designing with the Sun. Ria Stein. 2014.
- J. Uttley, Power Analysis, Sample Size, and Assessment of Statistical Assumptions-Improving the Evidential Value of Lighting Research, LEUKOS 15 (2019) 143-162. https://doi.org/10.1080/15502724.2018.1533851
Copyright © 2024 The Author(s). Published by solarlits.com.
 HOME
HOME Figure 1
Figure 1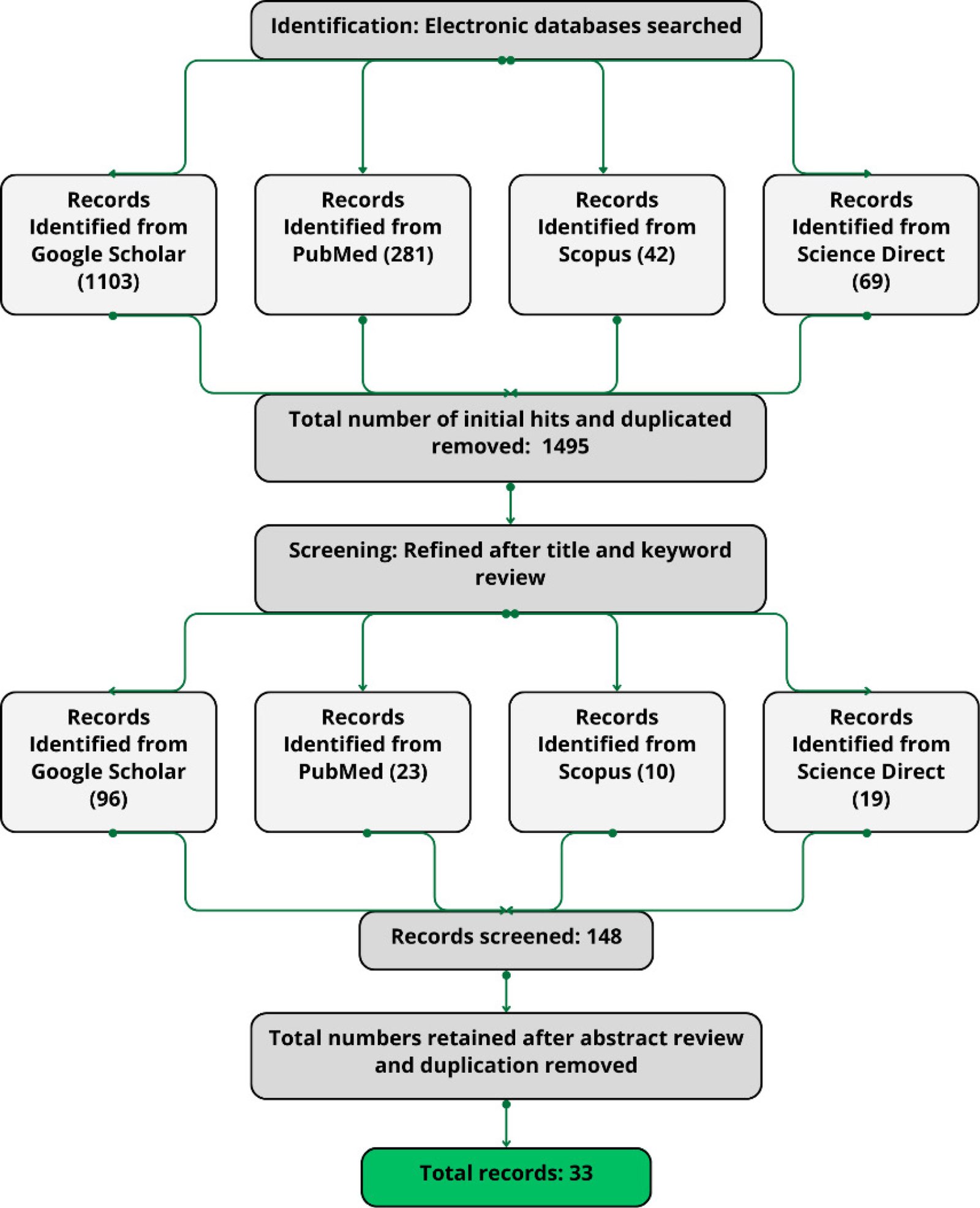 Figure 2
Figure 2 Table 1
Table 1 Table 2
Table 2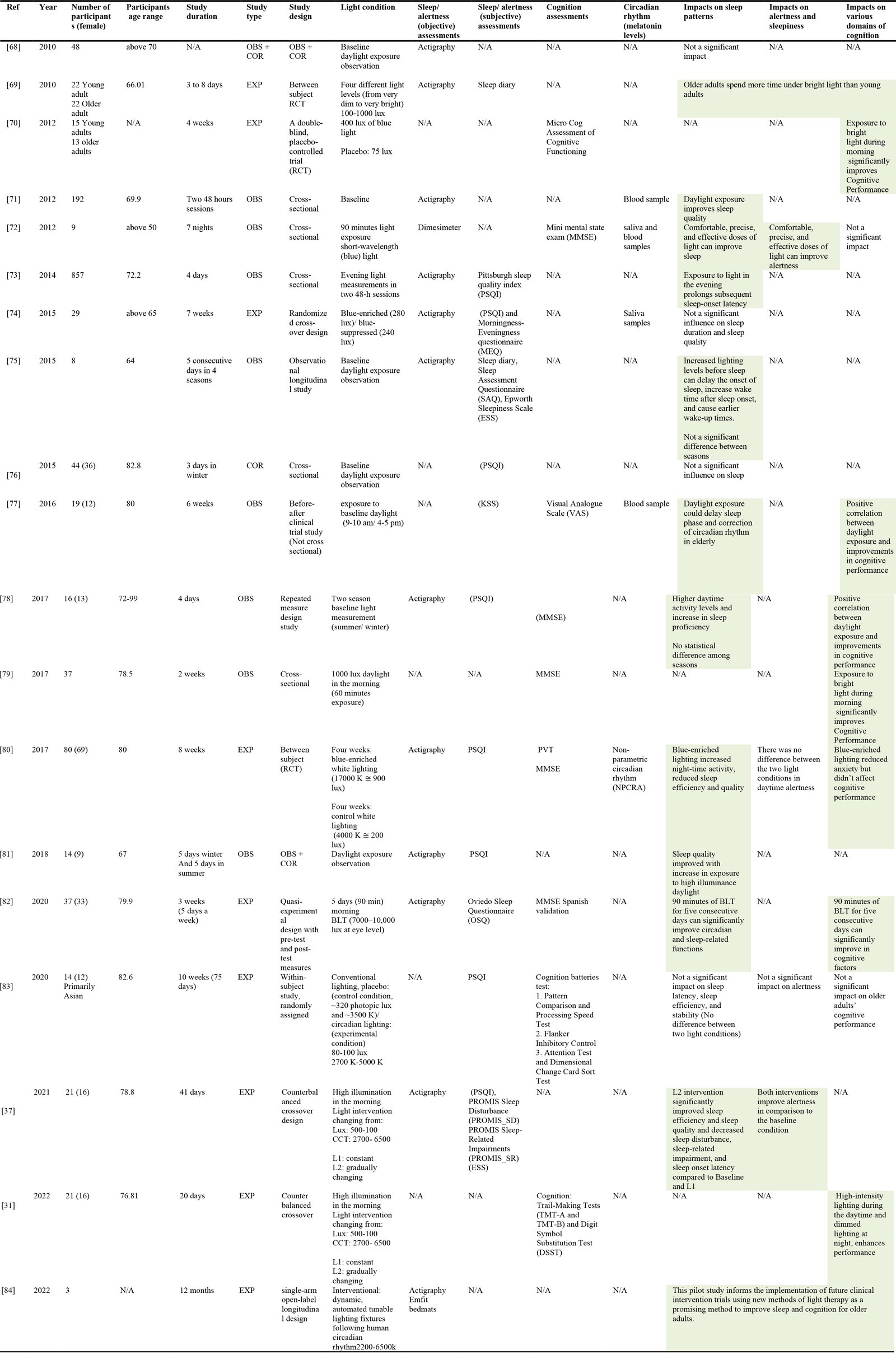 Table 3
Table 3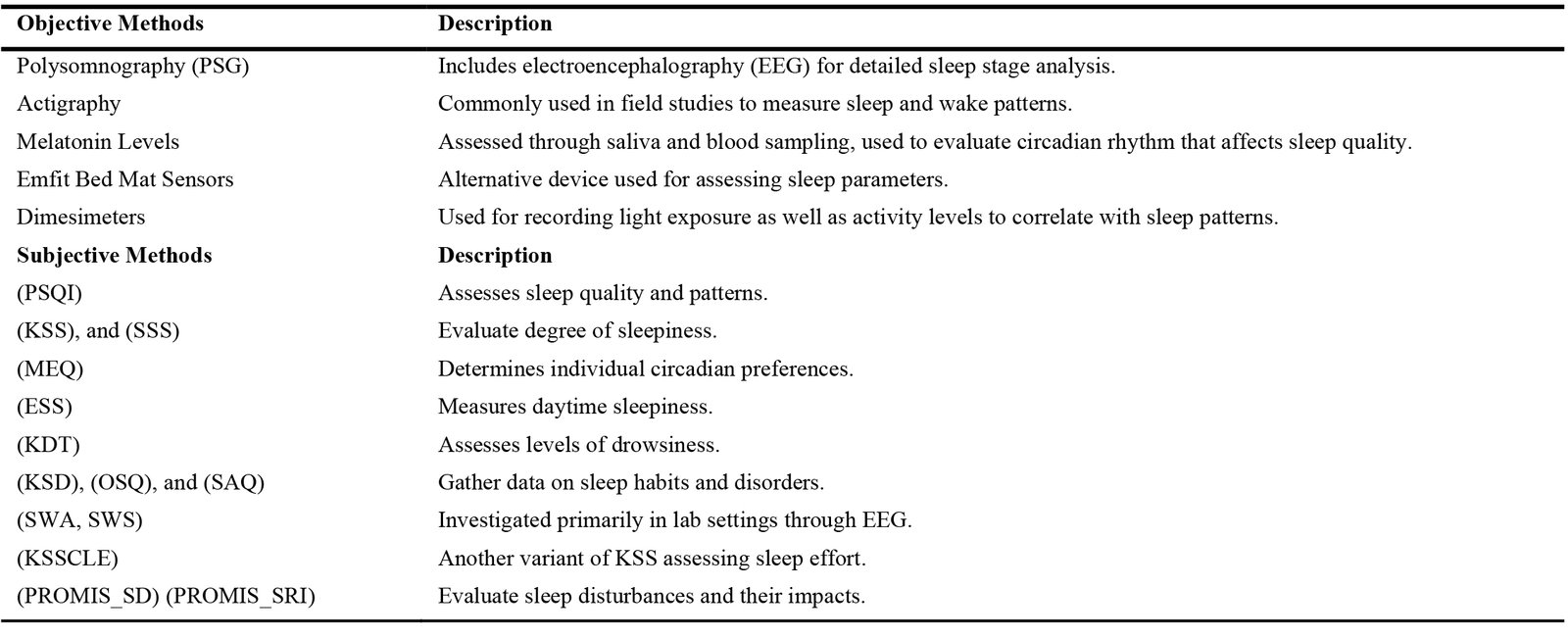 Table 4
Table 4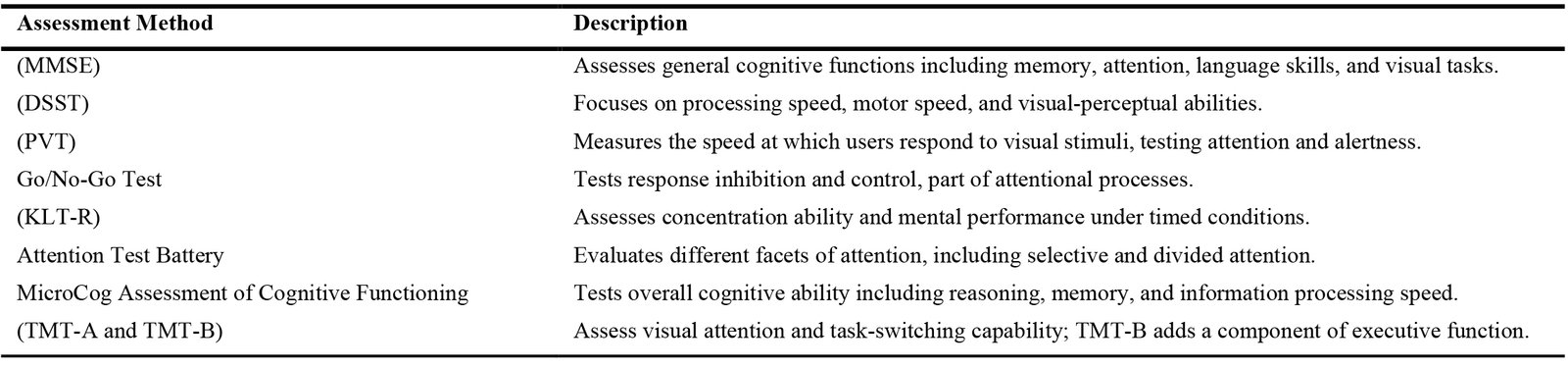 Table 5
Table 5


